Peritoneal Dialysis (PD) is a patient-centric therapy. Patient-centric approaches have been shown to empower patients, enhance their well-being, improve the quality of care, and add to health systems’ sustainability.1 In 2020 world-wide around 413,000 patients suffering from End Stage Kidney Disease were treated with Peritoneal Dialysis (PD) with increasing numbers.2
In addition to being treated at home, offering PD to patients has different benefits:
- Better preservation of residual kidney function than HD3,4
- No need to establish vascular access (e.g. fistula or graft)3,4
- Dialysis at home offers patients independence and scheduling flexibilty
- Less time spent travelling to and in dialysis facilities5,6
- Organize one’s life around dialysis and particularly ability to travel6
- PD has the same survival rate as conventional HD. Incident patients may even benefit from starting on peritoneal dialysis within the first years of dialysis6,7
CAPD: Individual clinical solutions for tailoring your patients’ therapy
In the area of Continuous Ambulatory Peritoneal dialysis (CAPD) our individual clinical solutions are designed for tailoring your patients’ therapy. The CAPD treatment stay•safe system contains the safety features DISC and PIN, which are connected with the PD fluids. The stay•safe system – small details that make a big difference.

PIN and stay•safe DISC technology have been designed for easy training of patients and to make treatment more convenient

with the stay•safe DISC which guides patients through their dialysis

with a unique PIN that closes the catheter extension before disconnection8
The guided operation is designed to increase patient compliance and reduce handling errors
The stay•safe Organizer brings together all parts of the system that your patients need for treatment

Patients can enjoy the benefits of the stay•safe CAPD therapy option in many countries enabling convenient travelling

Commitment to environmental sustainability by offering "PVC-free" and plasticiser-free system components (fluid bag, drainage bag and tubes) that are made from materials such as Biofine

Nordic Ecolabelling has certified various Fresenius Medical Care disposable Peritoneal Dialysis products
APD: Personalized treatment and adaptable over time
As individual as your patients: sleep•safe harmony
How can one cycler offer therapy options tailored to your patients’ needs?
In a small usability study from Reitz et al. the sleep•safe harmony cycler demonstrated good learnability and ease of use.9
Adapted APD (aAPD) therapy with sleep•safe harmony enables you to combine sequences of short dwells and small fill volumes with long dwells and large fill volumes and varying glucose concentrations. This way of prescribing PD, proposed by Fischbach et al., may have the potential to improve ultrafiltration (UF) and clearance within one PD session.10
sleep•safe harmony offers:
- Personalized treatment which is adjusted to your patients’ needs. Treatment flexibility options with integrated FlexPoint technology
- Adapted APD therapy option which has been reported to improve ultrafiltration and clearance10,11
- Integrated on-screen animations giving guidance and facilitating setup12
- Guided prescription on the cycler and via PatientOnLine software supporting therapy management (must be purchased separately)
Diverse training support for PD
Getting started with CAPD
We support you with a range of specific trainings that lay the foundation for a confident start to therapy. And while everybody is preparing, we help to make sure that everything is up and running in your patients’ homes.
Train
- Clearly structured digital and non-digital trainings for nurses and patients to support you
- The real-life stay•safe MyTraining VR supports a smooth start to the treatment
- Nutritional trainings to sideline therapy start
Start
- A team of experts help to coordinate home setup
- Starter kit with information on how to set up a home unit for Healthcare Professionals (HCPs)
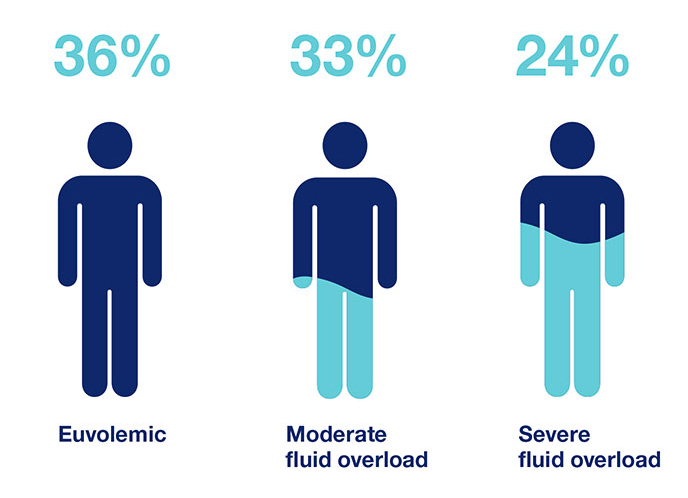
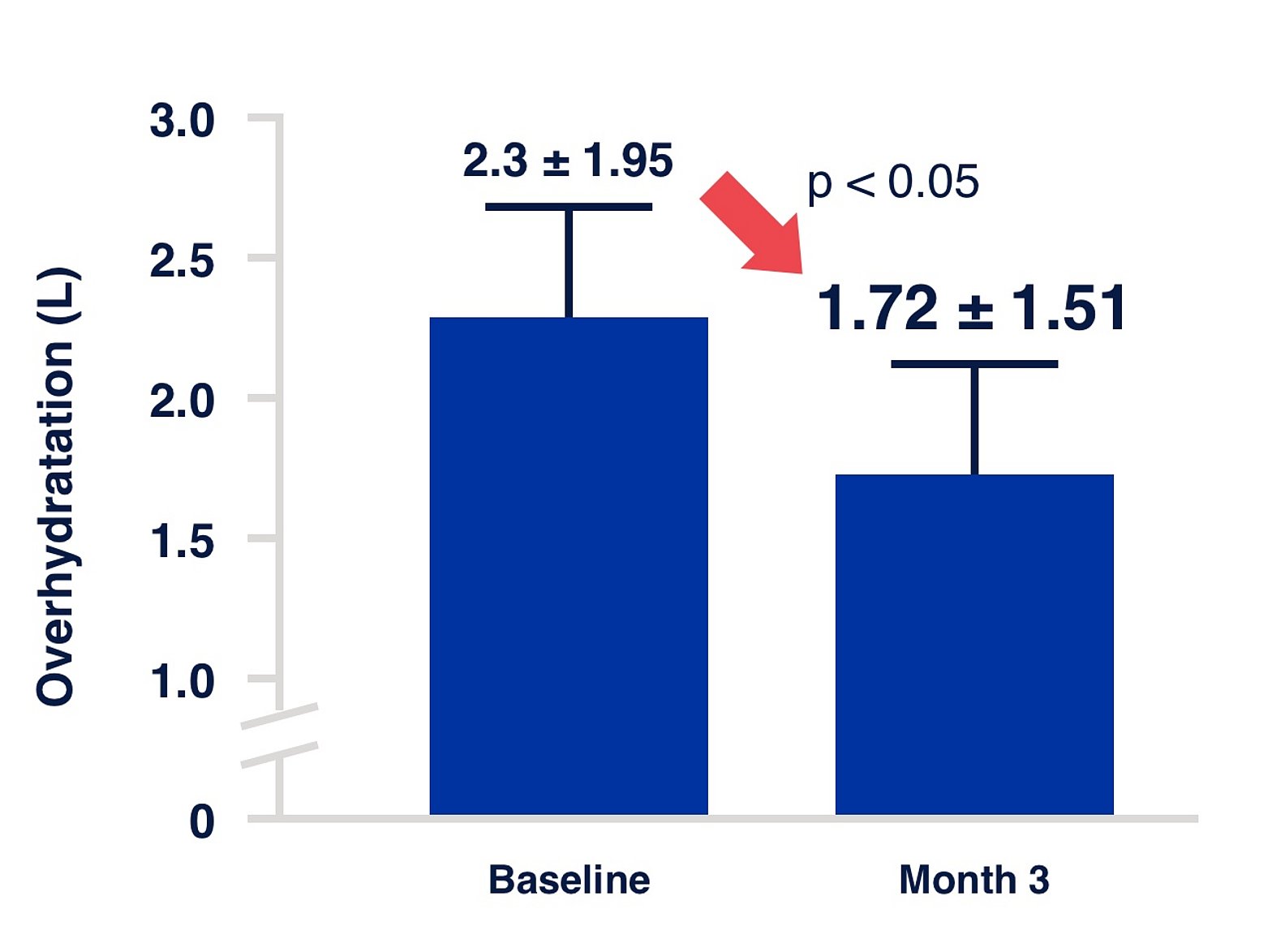
Figure 1:
Study information
Fluid status at the initiation of PD. Prospective cohort study implemented in 135 study centres across 28 countries.17 The IPOD-PD study has shown that fluid overload is already highly prevalent at the initiation of PD.18
Individualization of PD with fluid management
One of the major problems in today’s practice of renal replacement therapy is the quantitative assessment and management of fluid status. There are many factors known to affect fluid status such as comorbid conditions, medication, nutrition and treatment modalities.13,14
The treatment of fluid imbalance in dialysis patients is important because of its role in the development of cardiovascular (CV) diseases, which represent the leading cause of death in dialysis patients.15 Achieving euvolemia is hence a major goal in PD as both dehydration and overhydration can increase mortality through cardiovascular risk and impairment of residual kidney function (RRF).14,16
Important factors to consider in fluid status:
- UF alone can be misleading in evaluating patients’ fluid status.
- To improve a patient’s fluid volume status, both the inflow and outflow should be controlled.
- Blood pressure can be a misleading parameter to evaluate fluid status and can prompt false therapy decisions.
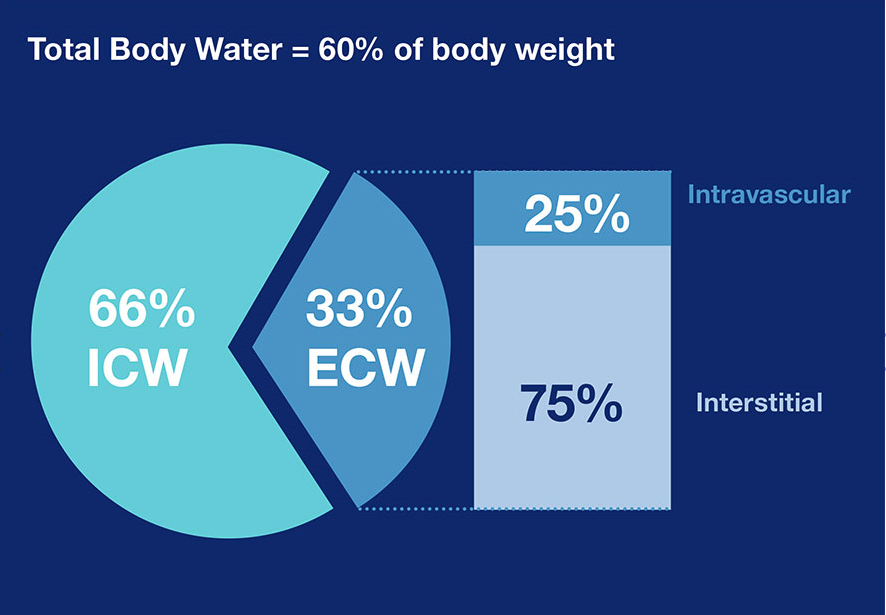
Figure 2: Distribution of TBW21
ISPD guidelines/ recommendations – Guideline on targets for solute and fluid removal in adult patients on chronic peritoneal dialysis
ISPD guidelines suggest that clinical assessment should include a diverse spectrum of clinical and laboratory results, including peritoneal and renal clearances, hydration status, appetite and nutritional status, energy level, hemoglobin concentration, responsiveness to erythropoietin therapy, electrolytes and acid–base balance, calcium phosphate homeostasis, and blood pressure control (Evidence level C).19
Fluid overload is triggered by the expansion of the extracellular water. When examining fluid overload, it is important to divide total body water (TBW) into intracellular (ICW) and extracellular water (ECW). The latter is further divided into circulating and interstitial compartments.20,21
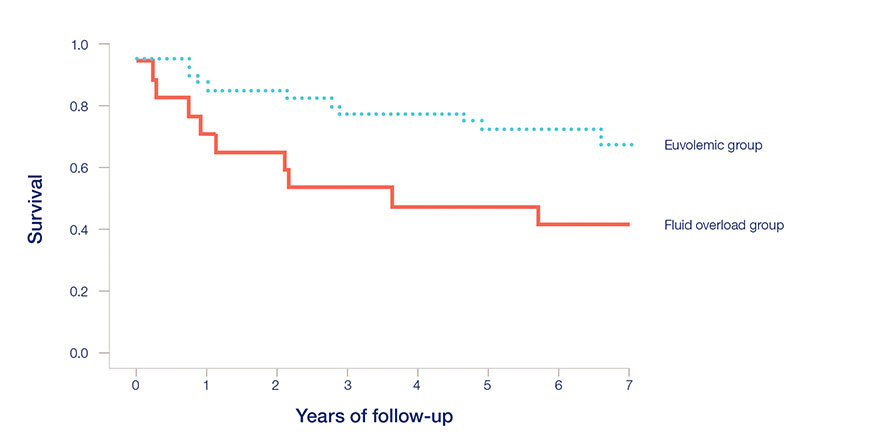
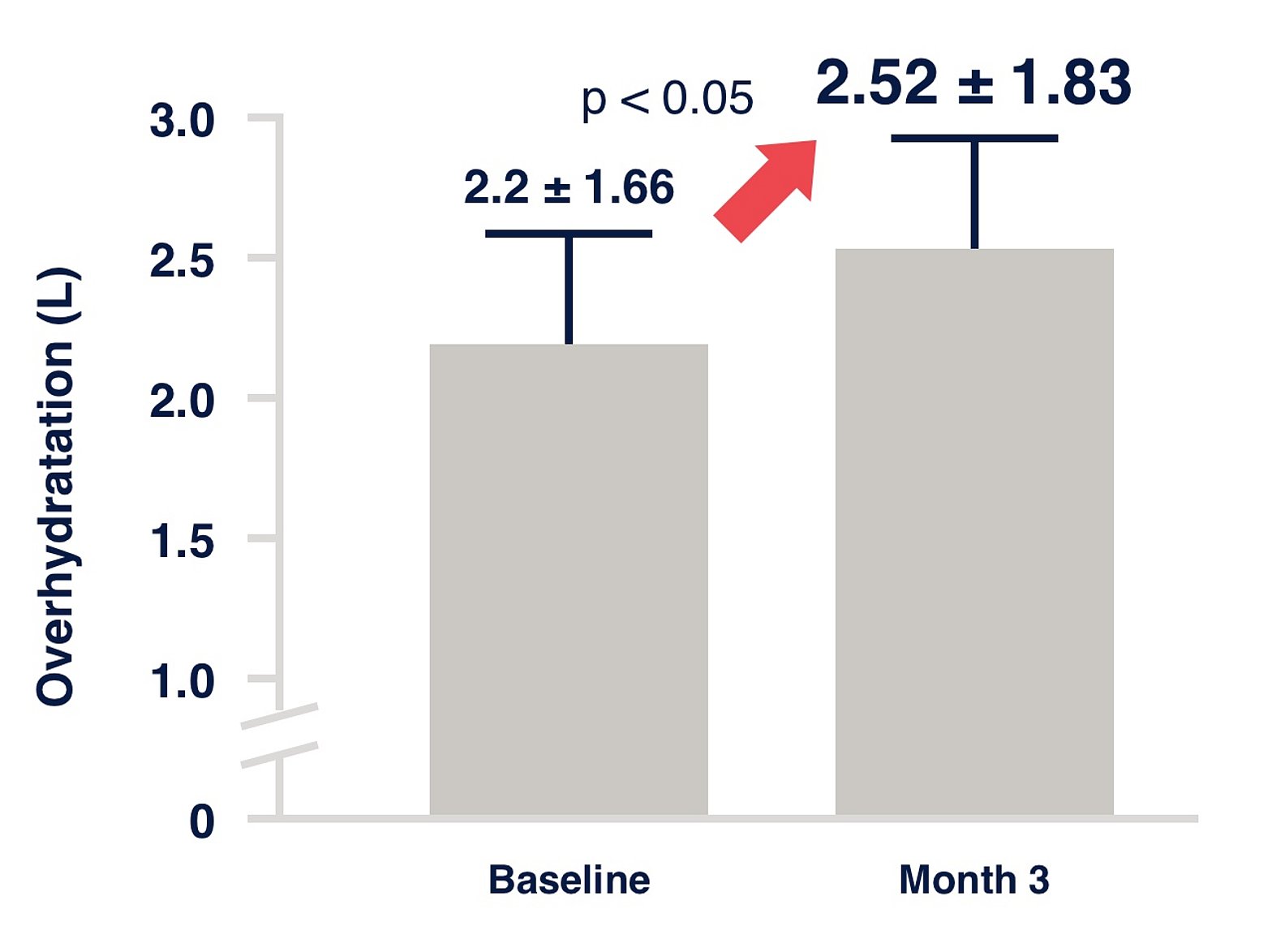
Figure 3:
Survival curves in euvolemic and fluid overloaded patients16
Study information
Single center, cross-sectional, oberservational study, followed up to 6.5 Years
Hydration measured by Body Composition Monitor
A step-by-step approach
A potential threat to the lives of Peritoneal Dialysis (PD) patients: fluid overload
Fluid management in peritoneal dialysis (PD) patients is highly important because it has been shown that:
- Fluid overloaded PD patients have a significantly higher mortality risk than euvolemic patients.16
Three steps for better fluid management
This step-by-step approach is designed to support your PD patients. Based on our experience and diverse portfolio, we provide solutions for every step of fluid management. Our products and services cover the entire process and offer the chance for improved patient outcome.

Experts from the International Society for Peritoneal Dialysis (ISPD) recommend the regular clinical assessment of fluid status.19
The BCM (Body Composition Monitor) is an addition to the routine evaluation of your patients and is actively used in many PD centers. It provides support for decision-making for the therapeutic management of volume control in PD patients. At every visit, you may assess and monitor your patients’ actual fluid status, allowing you to detect problems early and intervene with corrective measures.22
We recommend hydration status be assessed clinically on a regular basis during every follow-up visit and more often if clinically indicated.23
| Dehydration | Normohydration | Overhydration |
|---|---|---|
| Hypotension | Normotension | Hypertension |
| Loss of RRF | Preservation of RRF / Reduction of CV risk | Loss of RRF / LVH |
| Increased mortality | Improved survival | Increased mortality |
A rationale for better intake control
Excess intake of dietary sodium has detrimental effects on the health of PD patients. It raises extracellular osmolarity, leading to
- Movement of water from the intracellular compartment to the extracellular compartment, thereby resulting in volume expansion25
- Stimulation of thirst26
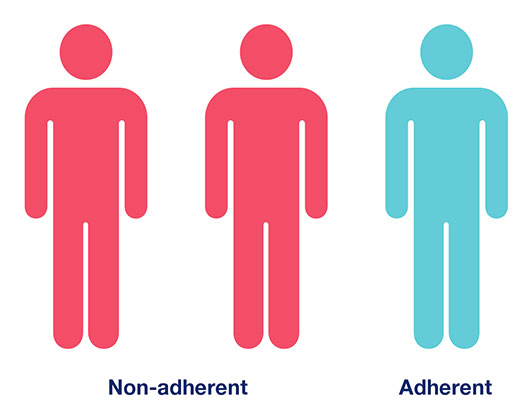
Despite the importance of this topic, a systematic review or peer-reviewed literature on adherence to dietary guidelines demonstrated that up to 67% of patients were found to be non-adherent.27
Therefore, further effort to improve the adherence of PD patients to dietary restriction of salt and fluid has to be spent. Any improvement in intake compliance would facilitate the overall correction of fluid imbalance.
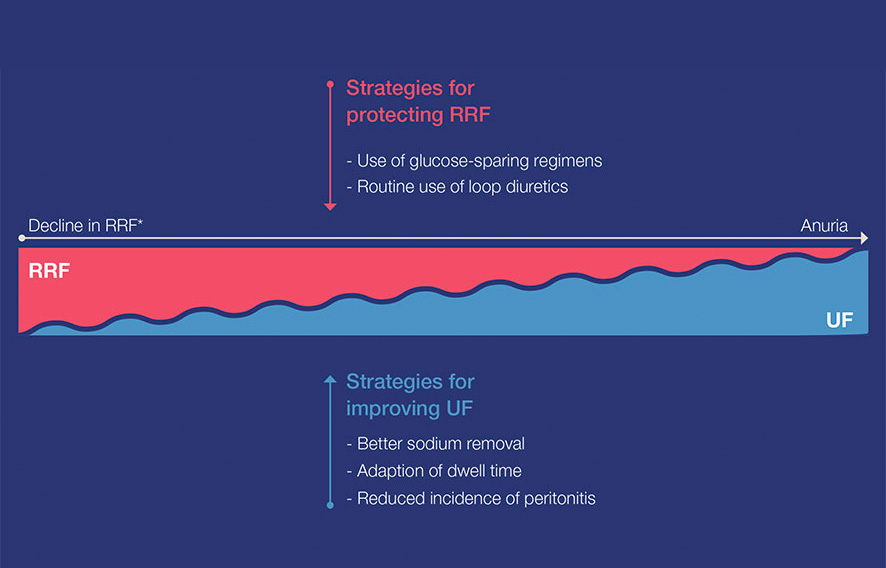
Figure 6: Figure illustrated the decline in RKF (fictional figure)
* Proposed model of the relationship between RKF and UF: simplified representation of the natural decline of RKF. The decline can vary greatly in individual patient cases.
Improving fluid output in PD patients
The contribution of the kidney
The decline of RKF impacts clinical outcomes. Loss of RKF not only triggers fluid overload, but also contributes to inflammation, anemia, malnutrition, LVH, hypertension and cardiovascular disease.28
The contribution of the technique
With the decrease of RKF in chronic kidney disease, ultrafiltration (UF) via PD becomes more important and challenging. PD allows an individualized dialysis prescription by combining different techniques, dialysis solutions and number and duration of dwells.17
In view of the importance of RKF and UF for successful fluid management, clinical strategies to preserving RKF and to improve UF are of paramount importance.
Maintain RKF and UF capacity to expand output
RKF is important for fluid and solute removal. Maintaining RKF is important for urine output and regulation of fluid status, thus using PD fluids may be an important contributor to your patient's fluid management.29
According to guidelines, it is recommended to use PD fluids that help to reduce the deleterious effects of chronic exposure to the peritoneal membrane and to preserve the membrane function longer.30,31,32
Important factors to consider in fluid status:
- UF alone can be misleading in evaluating patients’ fluid status
- Fluid status is mainly the result of the balance of intake and output over time. To improve a patient’s fluid status, both sides should be controlled in order to determine the fluid status trend13
- Blood pressure can be a misleading parameter to evaluate fluid status and can prompt false therapy decisions13
1 European Commission, Communication from the Commission to the European Parliament, The Council, The European Economic and Social Committee and the Committee of the Regions on enabling the digital transformation of health and care in the Digital Single Market 2018
2 Fresenius Medical Care, Annual Report 2020
3 Chan CT et al. Am J Kidney Dis 2019; 73(3):363-371
4 Auguste BL et al. Can J Kidney Health Dis 2019
5 Suri RS et al. Kidney Int. 2015; 88(2):360-8
6 Argilés A et al. Nephrology Dialysis Transplantation 2020; 35(11):1863-1839
7 Kumar VA et al. Kidney Int 2014; 86(5):1016-1022
8 Fresenius Medical Care, www.freseniusmedicalcare.asia/en/healthcare-professionals/home-therapies/staysafe-and-biofine/; 03/2022
9 Reitz T et al. Renal Replacement Therapy 2021; 7(20)
10 Fischbach M et al. Perit Dial Int 2011; 31(4):450-458
11 Vera M et al. PLoS One 2021; 16(12)
12 Punzalan S et al. Journal of Kidney Care 2017; 2(5):262-267
13 Ronco C et al. Contrib Nephrol 2012;178:164-168
14 Yong-Lim K et al. Seminars in Nephrol 2017; 37(1):43-53
15 Shu Y et al. Blood Purif 2018; 46(4):350-358
16 Jotterand Drepper V et al. PLoS One 2016; 11(7):e0158741
17 Van Biesen W et al. Clin J Am Soc Nephrol 2019; 14(6): 882-893
18 Ronco C et al. Nephrol Dial Transplant 2015; 30(5):849-858
19 Lo Wk et al. Perit Dial Int 2006; 26(5):520-522
20 Kim YL et al. Semin Nephrol 2017; 37(1):43-53
21 Chan et al. Eur J Comp Anim Pract 2014; 24:14-23
22 Cader RA et al. J Clin Nurs 2013; 22:741-748
23 Wang AY et al. Perit Dialysis Int 2015; 35:379-387
24 Luo YJ et al. Blood Purif 2011; 31:296-302
25 Wilson J et al. Semin Dial 2014; 17(4):260-4
26 Ahmad S et al. Semin Dial 2004; 17(4):284-7
27 Griva K et al. PLoS One 2014; 25;9(2):e8900
28 Marron B et al. Kidney Int Suppl 2008; 108:42-51
29 Xin L et al. Center for Kidney Diseases Nanjing Medical University 2016
30 Williams JD et al. Kidney Int 2004; 66(1):408-18
31 Weiss L et al. Perit Dial Int 2009; 29(6):630-633
32 Rippe B et al. Kidney Int 2001; 59(1):348-57