Volume control in peritoneal dialysis
A practical way to assess and help correct fluid status
- Quickly assess fluid status and recognize the trend
- Make therapeutic changes earlier
- Effortlessly use a wider range of practical volume control tools
Key features
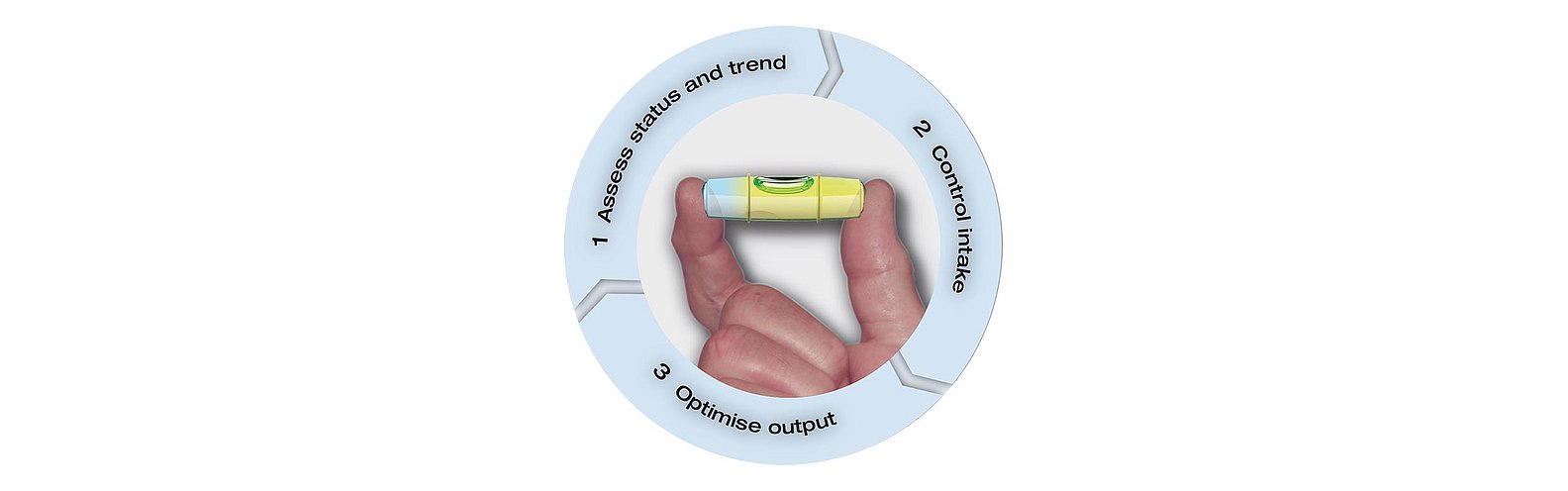
Volume control - three steps for better volume control
BCM-Body Composition Monitor
Assess status and trend
The easy-to-use BCM-Body Composition Monitor is a powerful addition to the routine evaluation of your patients and is becoming a standard in leading PD centers.
By providing you with a more precise picture of actual fluid status through quantified overhydration, this state-of-the-art technology helps you manage the fluid status of your patients better.
Analyze the fluid status trend
The BCM-Body Composition Monitor can be used effectively to continually monitor changes and trend of the fluid status over time. Trend analysis can provide important feedback and guidance on therapy decision-making by you and your staff.1
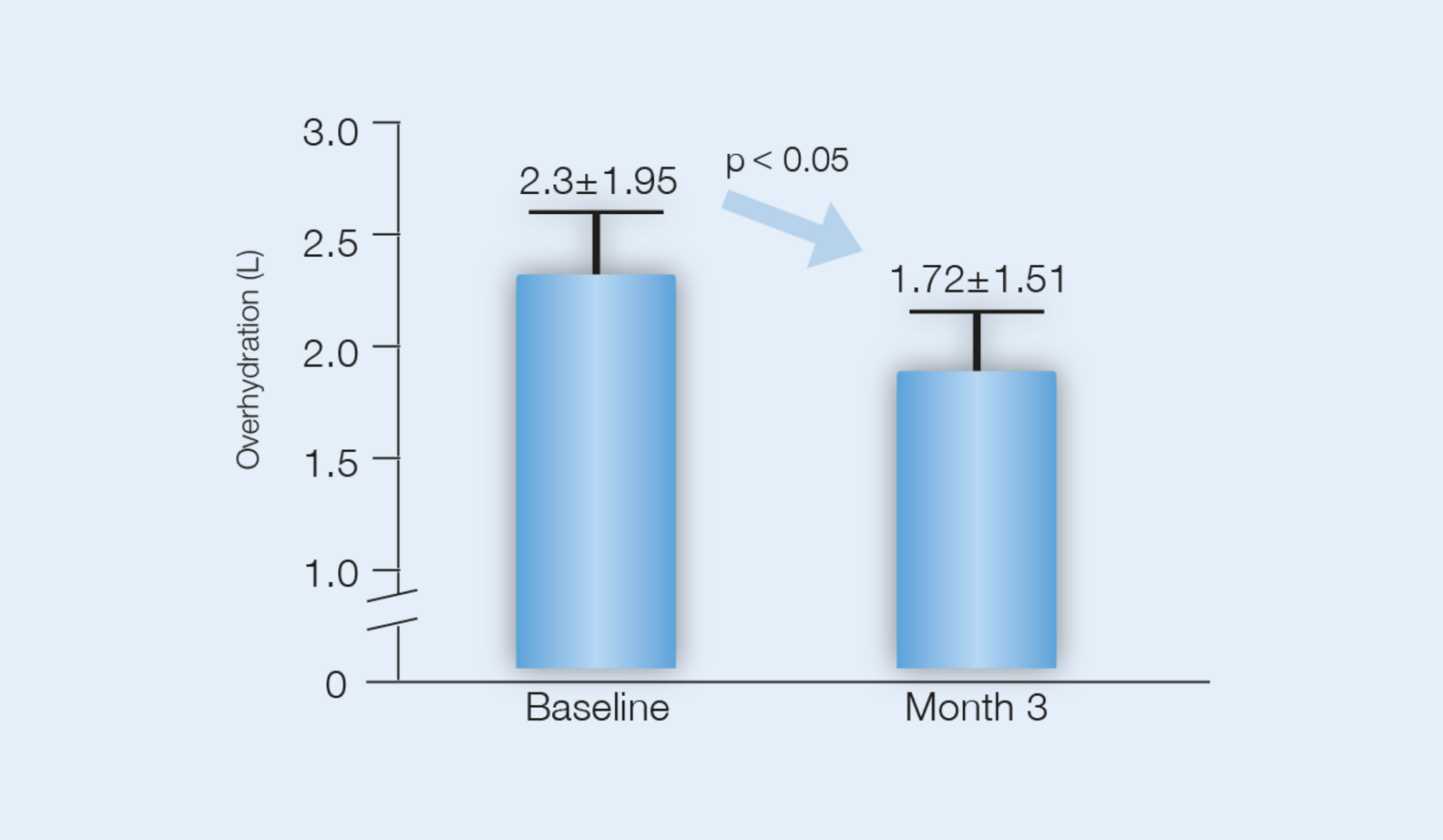
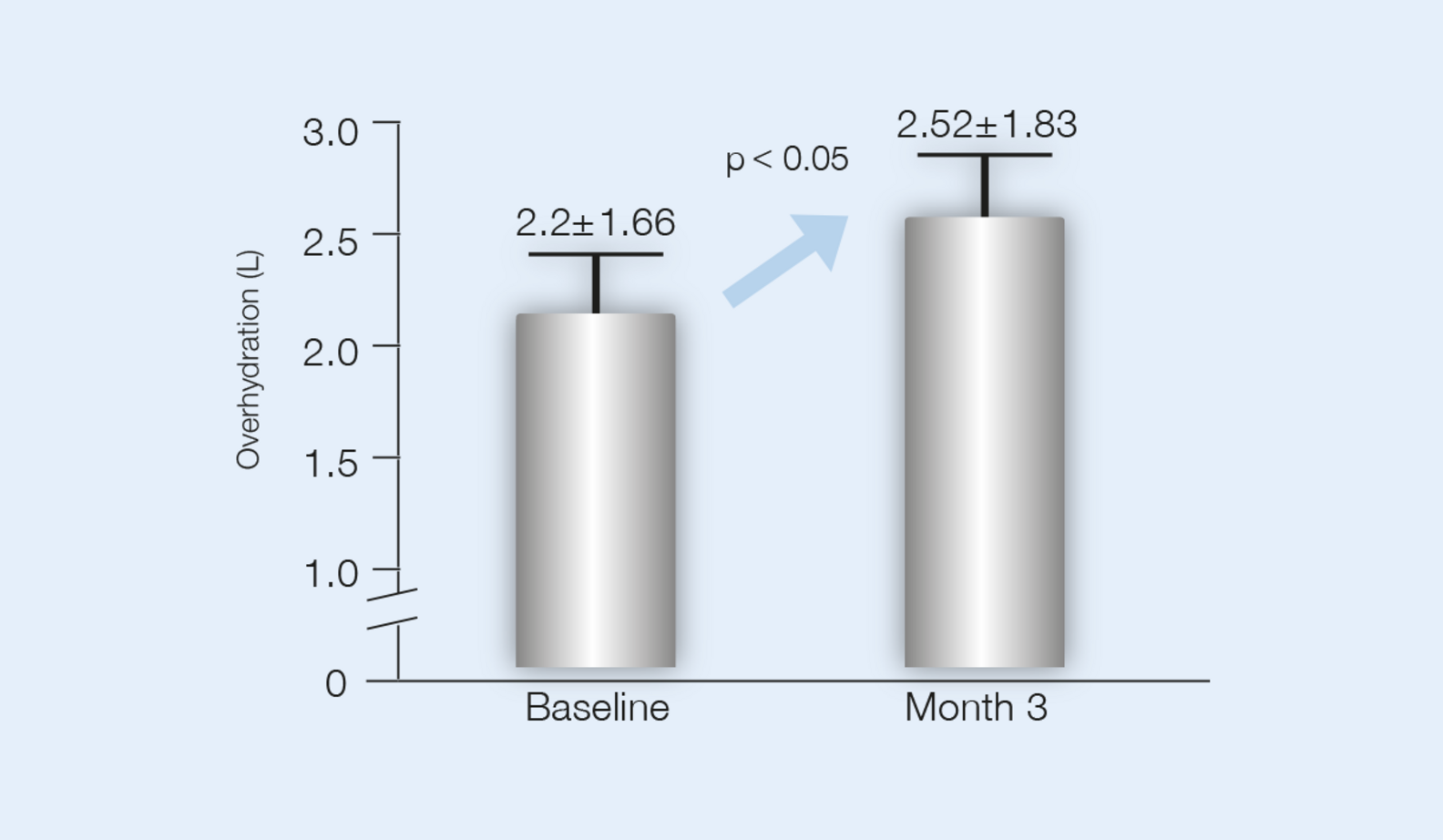
Volume status improvement as a result of awareness2
Evaluate fluid intake first
In the evaluation of the causes of fluid imbalance, screening for reversible causes first, is imperative. Any improvement in intake compliance facilitates the overall correction of fluid imbalance.
Use the power of awareness for better patient compliance. P3 Volume Control recommends an approach that is easy for your staff and even easier for your patients.
Improve fluid intake compliance
A randomized controlled study with the BCM-Body Composition Monitor showed conclusive results. Within three months of follow-up, patients who had knowledge of their fluid status, provided by the BCM-Body Composition Monitor, attained significantly better volume control. As a result, instances of overhydration decreased simply by raising patient awareness.2
Optimize output
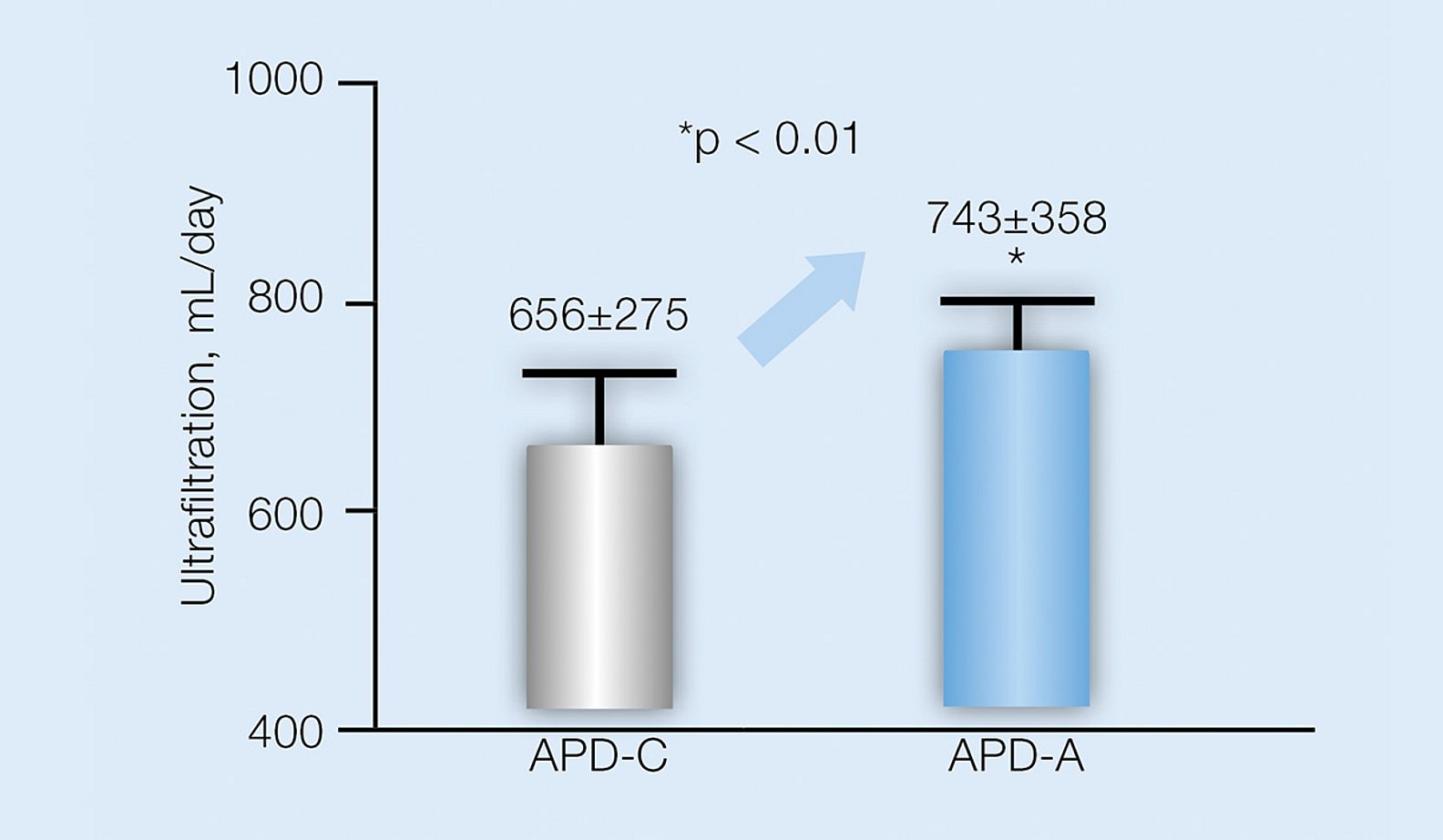
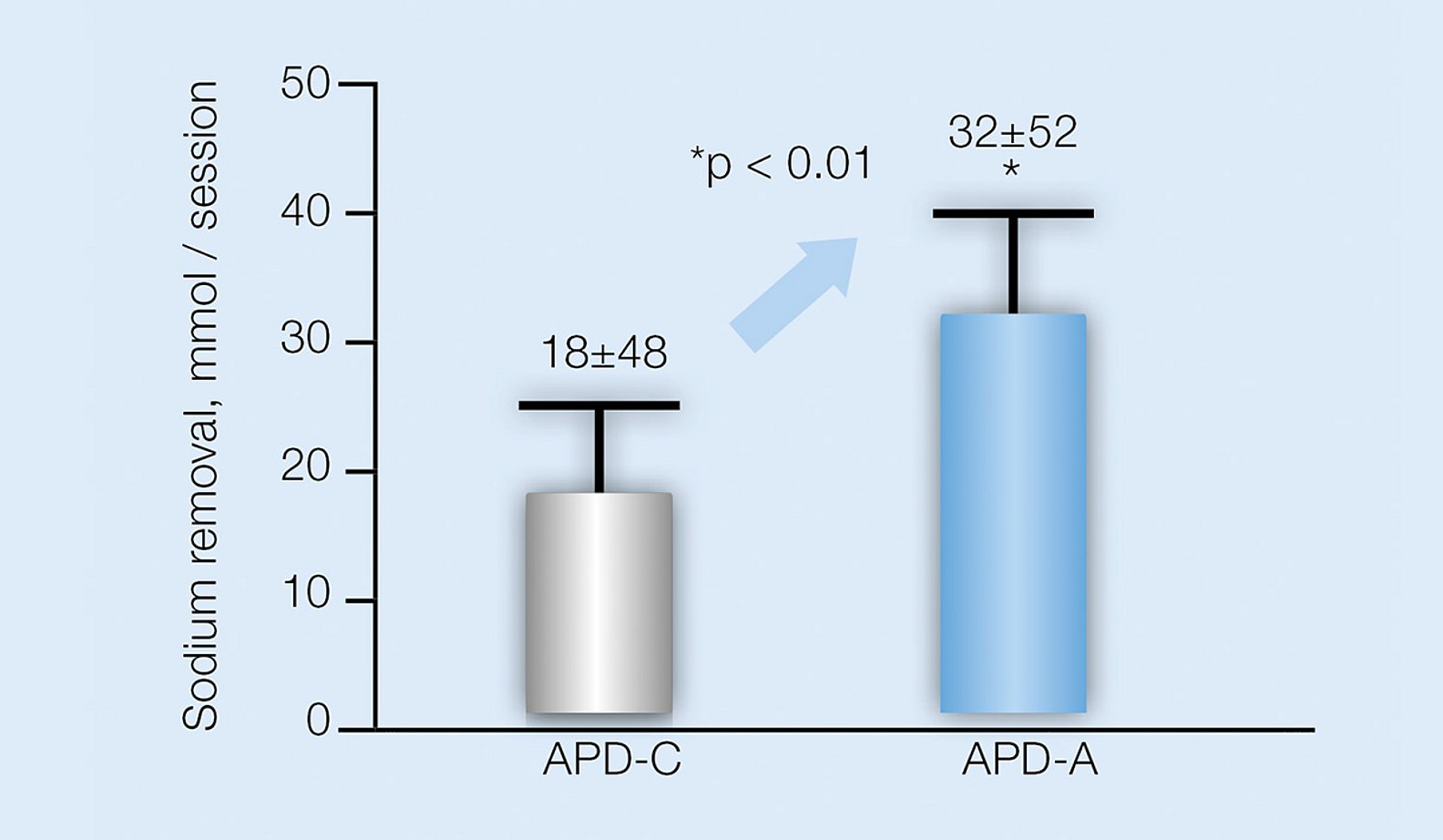
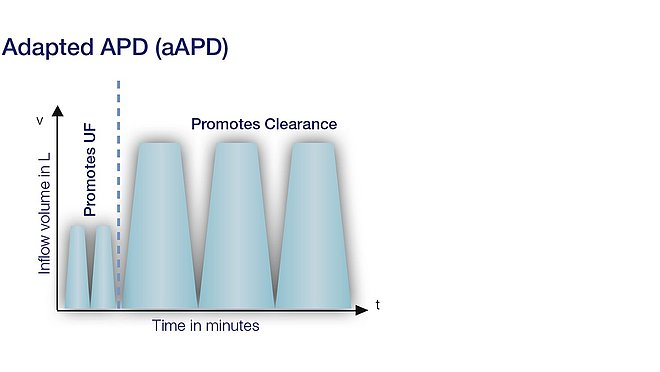
Adapted PD promotes both the process of UF and clearance
Adapted PD
By combining sequences of short dwell times and small fill volumes with long dwell times and large fill volumes, adapted PD promotes both the process of UF and clearance, at no additional time and cost, while reducing glucose absorption over the dialysis session.3
Maintain RRF and UF capacity to maximize output
RRF is important for fluid removal. Studies confirm that RRF can be preserved longer in patients using ultra-low GDP PD fluids compared to conventional PD fluids.4,5
4,5 Ultra-low GDP PD fluids can also help to reduce the deleterious effects of chronic exposure to the peritoneal membrane and to preserve the membrane function longer.6,7,8
Maintaining RRF is important for urine output and regulation of fluid status, thus the use of ultra-low GDP fluids can be an important part of your patient’s fluid management.
Studies
EuroBCM Study maintaining euvolemia in PD
EuroBCM Study results1
Out of 639 patients from 28 centers in 6 countries:
- 40% were normohydrated
- 7% were dehydrated
- 53% were overhydrated
Important factors to consider in fluid status:
- UF alone can be misleading in evaluating patients’ fluid status
- Fluid status is mainly the result of the balance of intake and output over time. To improve a patient’s fluid status, both sides should be controlled in order to determine the fluid status trend
- Blood pressure can be a misleading parameter to evaluate fluid status and can prompt false therapy decisions
Fluid status is mainly the result of the balance of intake and output over time

1 Van Biesen W, Williams JD, Covic AC, Fan S, Claes K, et al. (2011) Fluid Status in Peritoneal Dialysis Patients: The European Body Composition Monitoring (EuroBCM) Study Cohort. PLoS ONE 6(2): e17148. doi:10.1371/journal.pone.0017148
2 Luo Y, Lu X, Woods F, Wang T. Volume Control in Peritoneal Dialysis Patients Guided by Bioimpedance Spectroscopy Assessment. Blood Purification 2011;31:296-302.
3 Fischbach M, Issad B, Dubois V, and Taamma R. The beneficial influence on the effectiveness of automated peritoneal dialysis of varying the dwell time (short/long) and fill volume (small/large): randomized controlled trial. Peritoneal Dialysis International 2011; 31(4):450-8.
4 Kim S, Oh J, Kim S, Chung W, Ahn C, Kim SG, Oh KH. Benefits of biocompatible PD fluid for preservation of residual renal function in incident CAPD patients: a 1-year study. Nephrol Dial Transplant 2009;24(9):2899-90.
5 Haag-Weber M, Krämer R, Haake R, Islam MS, Prischl F, Haug U, Nabut JL, Deppisch R. Low-GDP fluid (Gambrosol trio) attenuates decline of residual renal function in PD patients: a prospective randomized study. On behalf of the DIUREST Study Group. Nephrology Dialysis Transplantation 2010;25(7):2288-96.
6 Williams JD, Topley N, Craig KJ, Mackenzie RK, Pischetsrieder M, Lage C,Passlick-Deetjen J; Euro Balance Trial Group. The Euro-Balance Trial: the effect of a new biocompatible peritoneal dialysis fluid (balance) on the peritoneal membrane. Kidney International 2004;66(1):408-18.
7 Weiss L, Stegmayr B, Malmsten G, Tejde M, Hadimeri H, Siegert CE, Ahlmén J, Larsson R, Ingman B, Simonsen O, van Hamersvelt HW, Johansson AC, Hylander B, Mayr M, Nilsson PH, Andersson PO, De los Rios T. Biocompatibility and tolerability of a purely bicarbonate-buffered peritoneal dialysis solution. Peritoneal Dialysis International 2009;29(6):630-633.
8 Rippe B, Simonsen O, Heimbürger O, Christensson A, Haraldsson B, et al. Long-term clinical effects of a peritoneal dialysis fluid with less glucose degradation products. Kidney International 2001;59(1):348-57.